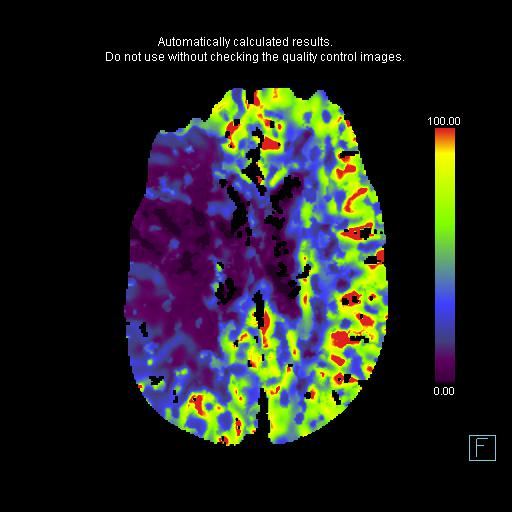
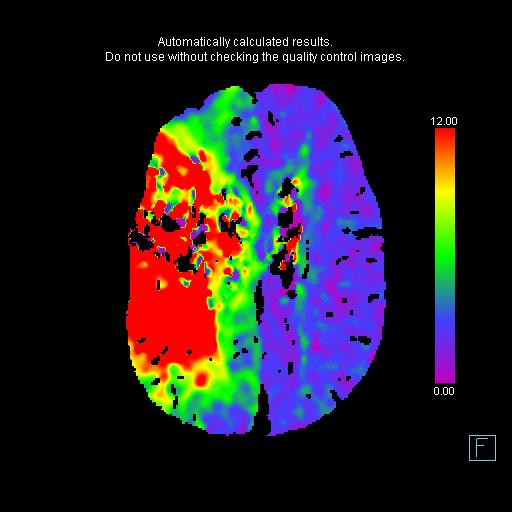
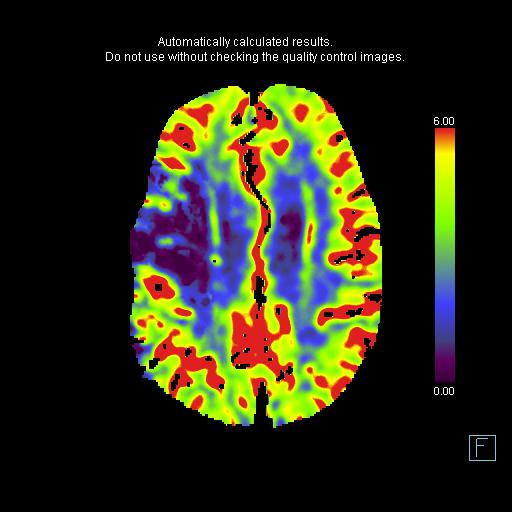
All interventional trials have used CBF to define the ischemic core and TMAX to define the ischemic at risk parenchyma. Using that convention, this is a matched defect without penumbra (this case was before the era of RAPID and if you use the older convention of CBV for ischemic core and CBF for at risk parenchyma, the core is smaller than the at risk parenchyma and the patient would be considered for intervention).
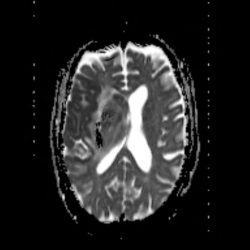
Interpreting the CTA is tricky. There is for sure a right carotid terminus occlusion as you can see the abrupt cut off of both right PCoM and right ACoM (in addition to seeing the strong evidence for clot on non-con CT). While there is lack of opacification of the right cervical ICA shortly after the bifurcation (orange arrow), this can be entirely flow related due to the upstream occlusion and resultant extremely slow flow.
Bonus: There is also PE, as discussed in the Readout.
There is PE also and thrombus in right subclavian
Thank you for your comment. There is indeed PE, I mentioned it in the Readout but not in the Discussion so I fixed that. Your assessment about the right subclavian having thrombus is incorrect, however. This is a left sided venous injection and so the left IJ, right IJ and right subclavian are unopacified as expected on this arterial phase CTA (not thrombosed). There is corresponding mixing artifact in the superior vena cava when the unopacified right subclavian vein and the opacified left subclavian vein join.